The Quiet Hormone Most Men Notice Too Late
Most men don’t wake up one morning thinking about testosterone.
It usually enters the conversation quietly. You notice workouts feel heavier than they used to. You sleep a full night but still wake up tired. Motivation dips, patience shortens, and things that once felt easy now require effort. Nothing dramatic. Just a slow shift that’s hard to explain.
For a long time, many men blame age, work stress, or responsibility. And sometimes that’s true. But often, something deeper is happening under the surface, something hormonal, biological, and largely invisible.
Testosterone rarely announces its absence loudly. It fades subtly, and because the process is gradual, it’s easy to accept it as normal life.
When Strength Isn’t Just About Muscles
There’s a common belief that testosterone is only about muscle or masculinity. That idea misses the bigger picture.
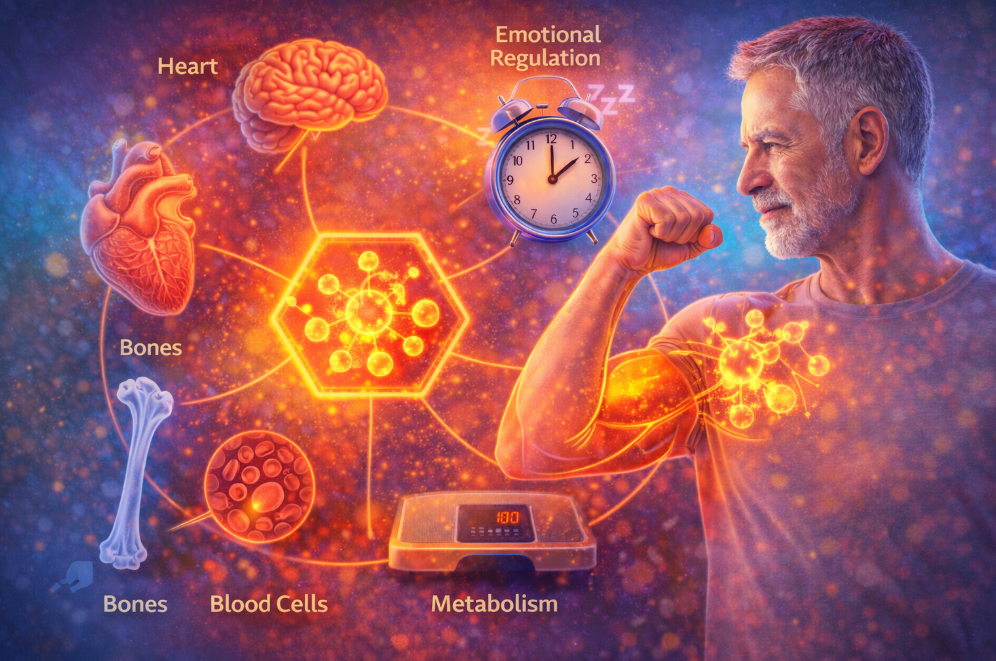
Testosterone quietly supports how the body holds itself together. It influences how energy is used, how bones stay strong, how blood cells are produced, and even how resilient the mind feels during stress. When levels are healthy, the body feels coordinated physically and mentally.
Doctors at institutions like the Cleveland Clinic often point out that hormones don’t work in isolation. Testosterone interacts with sleep cycles, metabolism, emotional regulation, and recovery. It’s less like a single switch and more like a background system keeping everything in rhythm.
When that rhythm changes, the effects ripple outward.
The Slow Shift Most Men Don’t Track
Testosterone levels don’t crash overnight. They drift.
Many men begin adulthood with robust levels, usually peaking in their late teens or early twenties. From there, levels often decline gradually. Not enough to feel dramatic year to year, but enough to accumulate over decades.
Long-term observational research discussed by the National Institute on Aging shows that this decline is common, but not identical for everyone. Some men maintain relatively stable levels well into later life. Others experience sharper drops earlier, often without understanding why.
What’s important is this: aging alone doesn’t tell the full story.
Modern Life Is Not Hormone Friendly
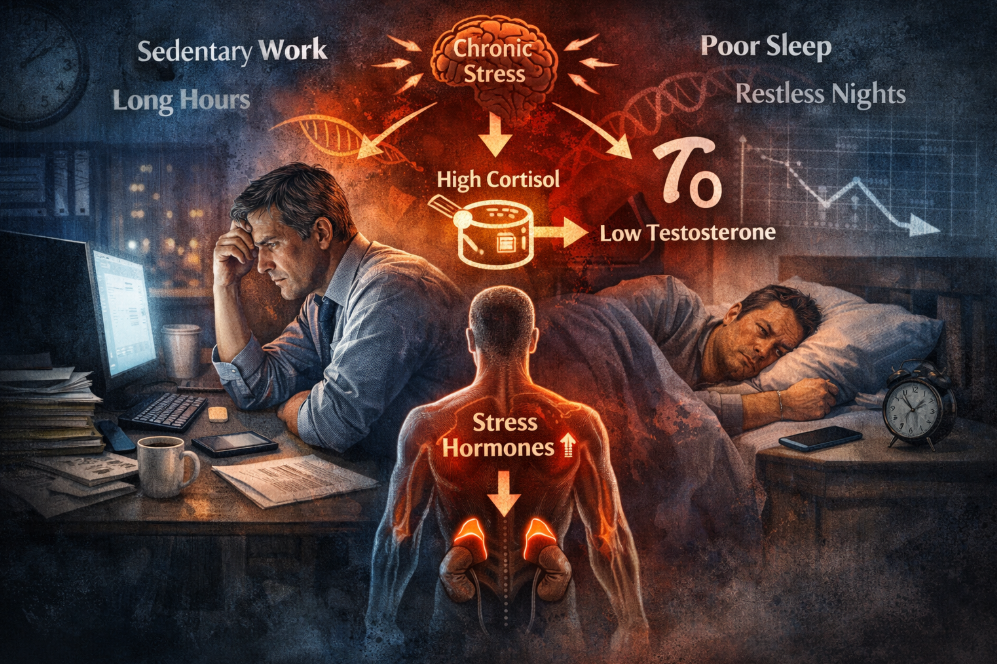
The way people live today is very different from how bodies evolved to function.
Movement has been replaced by sitting. Physical labour by screens. Stress no longer comes in short bursts but lingers constantly in the background. Sleep is often fragmented, interrupted, or treated as optional.
Harvard Health researchers have frequently highlighted that chronic stress alone can interfere with hormonal balance. Elevated stress hormones quietly suppress testosterone production. Add poor sleep and long workdays, and the body begins prioritising survival over optimisation.
It’s not that the body is failing, it’s adapting to what it perceives as ongoing pressure.
Fatigue That Sleep Doesn’t Fix
One of the earliest signs men describe isn’t weakness, it’s exhaustion.
Not the kind that comes from a long day, but the kind that lingers. The body feels heavy. Recovery takes longer. Even motivation feels physically depleted.
Endocrinologists often explain that testosterone supports efficient energy use. When levels decline, the body becomes less economical. Everything costs more effort mentally and physically.
This is why fatigue linked to low testosterone often feels different from ordinary tiredness. Rest helps, but never quite enough.
Weight Gain That Feels Unfair
Another quiet change many men notice is weight gain that doesn’t respond the way it used to.
The same meals. The same activity. Different results.
Testosterone plays a role in how the body partitions energy whether calories are directed toward muscle maintenance or stored as fat. As levels drop, muscle mass becomes harder to maintain, and fat storage becomes easier.
Global health discussions published through organisations like the World Health Organization frequently emphasise that body composition is hormonally regulated. Willpower alone doesn’t override biology.
This explains why some men feel as though their bodies are suddenly working against them.
Mood, Confidence, and the Inner Landscape
Testosterone doesn’t just affect the body. It shapes how the mind responds to life.
Men with declining levels often describe feeling less driven, more irritable, or emotionally flat. Confidence doesn’t vanish, but it dulls. Stress feels heavier. Motivation feels forced.
Psychological research discussed by universities such as King’s College London has explored how hormones influence neurotransmitters involved in mood regulation. Testosterone appears to support emotional resilience, especially during prolonged stress.
This doesn’t mean low testosterone causes depression but it can lower the buffer that helps men cope.
Sleep: Where Hormones Are Made or Missed
One of the least appreciated aspects of testosterone health is sleep.
Most daily testosterone release occurs during deep sleep. When sleep is short, fragmented, or inconsistent, production suffers.
Sleep specialists at Stanford Medicine have repeatedly shown that even short-term sleep restriction can noticeably reduce testosterone levels in healthy men. Over months or years, the effect compounds.
Late nights, screens before bed, irregular schedules they all send the same message to the body: now is not a safe time to invest in long-term maintenance.
Exercise: Not Extreme, Just Consistent
You don’t need to live in a gym to support testosterone.
In fact, excessive training without recovery can have the opposite effect.
What matters most is regular resistance giving muscles a reason to stay metabolically active. This can come from weights, body-weight exercises, carrying loads, or functional movements.
Sports medicine experts often explain that muscles communicate hormonally. When they are used, they send signals that support testosterone production. When they’re ignored, those signals weaken.
Consistency beats intensity every time.
Food Is Not Just Fuel, It’s Information
The body reads food as information.
Severely restricting calories, avoiding fats entirely, or skipping meals for long periods can signal scarcity. In response, the body conserves resources including hormone production.
Nutrition researchers writing for journals like The Lancet Diabetes & Endocrinology have noted that hormonal health depends on adequacy, not extremes.
Healthy fats, sufficient protein, and micronutrients like zinc and vitamin D quietly support testosterone synthesis. This doesn’t require perfection just balance.
Medical Testing and Reality
Low testosterone is not diagnosed by symptoms alone.
Blood tests, interpreted correctly and in context, provide clarity. Timing matters. Health history matters. Symptoms matter.
Clinicians at places like Mayo Clinic consistently stress that treatment decisions should never be based on numbers alone. The goal is not chasing youthful levels, but restoring functional balance.
This article is for informational purposes only and does not replace professional medical advice.
Aging Does Not Mean Decline Is Mandatory
Here’s the most important truth:
Aging changes the body, but it does not automatically mean losing strength, clarity, or vitality.
Men who prioritise movement, sleep, nourishment, and stress regulation often maintain healthier testosterone levels far longer than expected. Not because they fight aging but because they support adaptation.
Hormones respond to signals. When the body feels supported, it behaves differently.
Final Reflection
Testosterone is not about proving masculinity or chasing youth.
It’s about feeling steady in your body. Capable. Resilient. Clear-headed enough to meet life without constant friction.
The decline is quiet. So is the solution.
Small, repeated habits shape hormonal health far more than dramatic interventions. And understanding what’s happening beneath the surface is often the first step toward feeling like yourself again.
References
Harvard Health Publishing
Cleveland Clinic
Mayo Clinic
Stanford Medicine Sleep Center
National Institute on Aging
World Health Organization
The Lancet (Endocrinology & Metabolism)
King’s College London (Psychology & Neuroscience)

