For a long time, I barely thought about my prostate. Like many men, it simply wasn’t part of everyday conversation, routine health checks, or even casual curiosity. It wasn’t until I started reading more about men’s health, especially as I noticed how often prostate issues came up in medical discussions, that I realized how central this small gland is to overall well-being.
In this article, I want to share what I’ve learned about the prostate in a straightforward, educational way. This is not medical advice, but rather a well-researched overview based on trusted health sources in the United States. My goal is to help other men better understand what the prostate is, how it changes over time, and why paying attention to prostate health is important.

What Is the Prostate and Why Does It Matter?
The prostate is a small, walnut-sized gland located just below the bladder and in front of the rectum. I learned that it plays a role in the male reproductive system by producing fluid that becomes part of semen. This fluid helps nourish and transport sperm. (National Cancer Institute)
What surprised me most was how such a small gland can have such a noticeable impact on daily life, especially as men age. Because the prostate surrounds part of the urethra, the tube that carries urine from the bladder, even small changes in its size can affect urination. (National Institute on Aging)
How the Prostate Changes With Age
One thing that became clear in my research is that the prostate is not static. It naturally changes as men grow older. According to U.S. health agencies, prostate enlargement is common and often begins in midlife. (National Institute of Diabetes and Digestive and Kidney Diseases)
This doesn’t necessarily mean something is wrong. In fact, many men experience prostate changes without serious complications. Still, understanding these changes can help reduce anxiety and encourage timely conversations with healthcare providers.
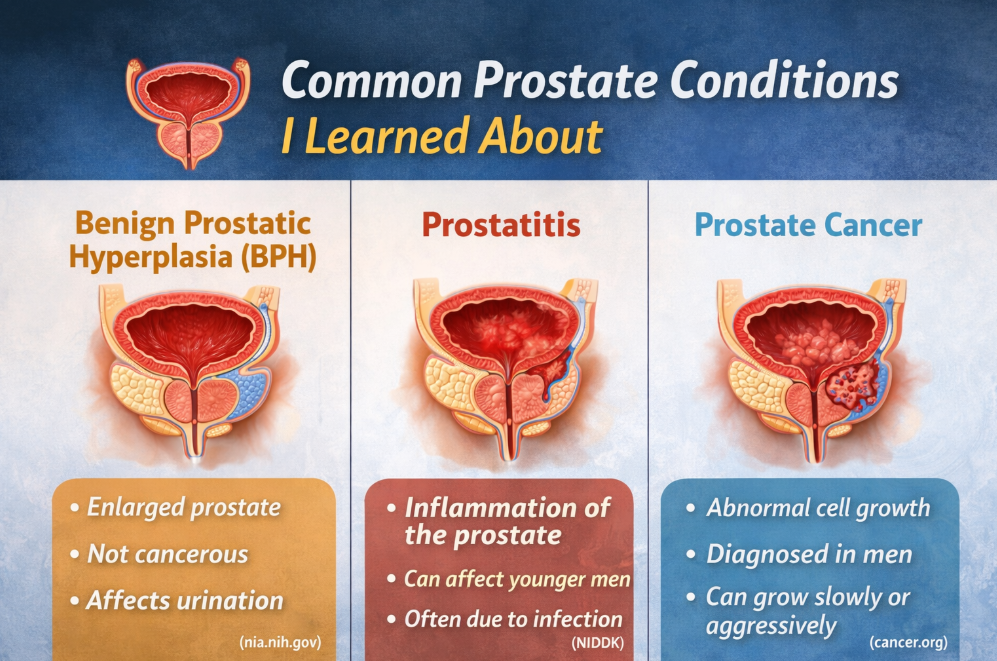
Common Prostate Conditions I Learned About
1. Benign Prostatic Hyperplasia (BPH)
One of the most common prostate conditions I came across is Benign Prostatic Hyperplasia, often shortened to BPH. Despite the intimidating name, “benign” means it is not cancer.
BPH refers to an enlarged prostate that can press against the urethra and affect urine flow. Commonly discussed symptoms include:
- Frequent need to urinate
- Difficulty starting urination
- Weak urine stream
- Feeling that the bladder hasn’t fully emptied
According to the National Institute on Aging, BPH becomes more common as men get older and is especially prevalent after age 50. (nia.nih.gov)
2. Prostatitis
Another condition I learned about is prostatitis, which refers to inflammation of the prostate. Unlike BPH, prostatitis can affect younger men as well. Some forms are caused by bacterial infections, while others have unclear causes. (NIDDK)
Symptoms discussed in medical literature may include pelvic discomfort, painful urination, or flu-like symptoms in acute cases. Treatment depends on the underlying cause and often involves medical evaluation. (NIDDK)
3. Prostate Cancer
Prostate cancer is one of the most talked-about prostate conditions, and understandably so. According to the American Cancer Society, it is among the most common cancers diagnosed in men in the United States. (cancer.org)
What stood out to me is that prostate cancer often grows slowly, and many men live long lives without symptoms or complications. However, some forms can be aggressive, which is why awareness and screening discussions matter.
Risk Factors That Are Commonly Discussed
While researching prostate health, I noticed recurring themes around risk factors. These don’t guarantee a condition will develop, but they may increase the likelihood according to U.S. health authorities:
- Age risk increases significantly after age 50
- Family history of having a close relative with prostate cancer may raise the risk
- Race and ethnicity african American men are statistically at higher risk for prostate cancer and more aggressive forms (CDC)
- Lifestyle factors research continues into the role of diet, activity, and overall health
Understanding risk factors helps contextualize why doctors recommend different screening approaches for different individuals.
Symptoms: Why They’re Not Always Obvious
One of the most important things I learned is that prostate conditions don’t always cause clear symptoms, especially in early stages. This is particularly true for prostate cancer. (National Cancer Institute)
When symptoms do appear, they may overlap across conditions, including urinary changes or pelvic discomfort. This overlap is one reason healthcare providers emphasize evaluation rather than self-diagnosis.
Prostate Screening: What I Learned About PSA Testing
The Prostate-Specific Antigen (PSA) test is often discussed in conversations about prostate health. PSA is a protein made by the prostate, and higher-than-normal levels in the blood can be associated with prostate conditions. (CDC)
What I found particularly important is that U.S. medical organizations stress shared decision-making. This means men should discuss the benefits and limitations of PSA testing with their healthcare providers rather than automatically undergoing screening. (U.S. Preventive Services Task Force)
Lifestyle and Prostate Health: Observations From Research
While no lifestyle choice can guarantee prostate health, many reputable sources suggest that general wellness habits support overall health, including the prostate:
- Balanced nutrition with fruits and vegetables
- Regular physical activity
- Maintaining a healthy weight
- Avoiding tobacco use
The National Cancer Institute notes ongoing research into how lifestyle patterns may influence prostate health, though definitive conclusions are still being studied. (cancer.gov)
Why Men Often Delay Talking About Prostate Health
One thing that struck me during my research is how often men delay discussing prostate concerns. Cultural discomfort, fear, or simply not noticing symptoms can all play a role. U.S. public health campaigns increasingly emphasize normalizing conversations about men’s health. (CDC)
From what I’ve read, early conversations, even without symptoms, can reduce stress and lead to better-informed decisions later in life.
Living With a Prostate Condition
Many men in the United States live full, active lives with prostate conditions. Management strategies vary widely depending on diagnosis and individual health factors. Options discussed by healthcare professionals may include monitoring, medication, or other interventions based on evidence-based guidelines. (NIDDK)
What stands out is that prostate conditions are not automatically emergencies, but they do deserve attention and professional guidance.
Why Education Matters
Learning about the prostate changed how I think about preventative health. Understanding basic anatomy, recognizing common conditions, and knowing when to seek professional input makes prostate health feel less intimidating and more manageable.
Reliable, reference-based information plays a critical role in countering misinformation, especially online, and empowers individuals to engage confidently with healthcare providers.
Final Thoughts
The prostate may be small, but its role in men’s health is significant. From normal age-related changes to more complex medical conditions, understanding the prostate helps men make informed, thoughtful decisions about their health. Open discussions, regular checkups, and evidence-based information are essential steps toward long-term well-being.
This article is for informational purposes only and does not replace professional medical advice.

